Introduction
Glaucoma, known as the ‘Silent Thief of Sight’, frequently progresses undetected, resulting in substantial visual loss.
Glaucoma eye conditions are notorious for damaging the optic nerve, which is vital for vision, leading to gradual deterioration and potentially resulting in blindness if left undiagnosed. Glaucoma’s harmful nature and profound implications highlight the need for awareness, early detection, and proactive management.
Here’s a closer look at some of the primary causes of Glaucoma.
Causes:
Heredity
Genetics significantly elevate the risk of Glaucoma, implicating eye pressure, optic nerve sensitivity, and drainage system integrity. Individuals with a family history of Glaucoma should have regular eye examinations for early detection and more effective treatment.
Diabetes
Diabetes is an underlying condition that can impact the eyes. It elevates the risk for Glaucoma, particularly Neovascular Glaucoma, a severe form triggered by abnormal blood vessel growth. Changes in retinal blood vessels can lead to diabetic retinopathy and Glaucoma, emphasising the crucial connection between blood sugar management and eye health. Maintaining blood sugar levels and having periodic eye examinations are essential ways to avoid vision-related concerns.
Age
Age is a significant risk factor for Glaucoma, especially past 40. With advanced age, the eye’s drainage system may become less efficient, increasing Intraocular Pressure and risking Glaucoma. Annual comprehensive eye exams are essential for early detection and treatment.
Myopia
Myopia increases the risk of Glaucoma. Though the exact cause is uncertain, structural changes in myopic eyes, such as increased eye length, are thought to contribute to Glaucoma. Myopic people need regular eye exams to identify eye issues.
Symptoms:
Symptoms of Glaucoma, the ‘Silent Thief of Vision’, can be challenging to diagnose, particularly in the early stages of Primary Open-angle Glaucoma, the most prevalent kind. Acute Angle-Closure Glaucoma (AACG) is less common but more severe and may intensify quickly, necessitating emergency medical intervention.
Symptoms of AACG:
- Severe Eye Pain: An intense, throbbing pain in the eye may also be accompanied by headache, nausea, and vomiting.
- Redness: The eye appears noticeably red, indicating irritation or increased pressure.
- Blurred Vision: Vision suddenly becomes blurred or hazy, often accompanied by halos around lights.
- Seeing Halos Around Lights: A visual phenomenon where bright circles appear around light.
- Nausea and Vomiting: The extreme pain from AACG can cause systemic symptoms such as nausea and vomiting.
A Multi-Faceted Approach to Glaucoma Assessment
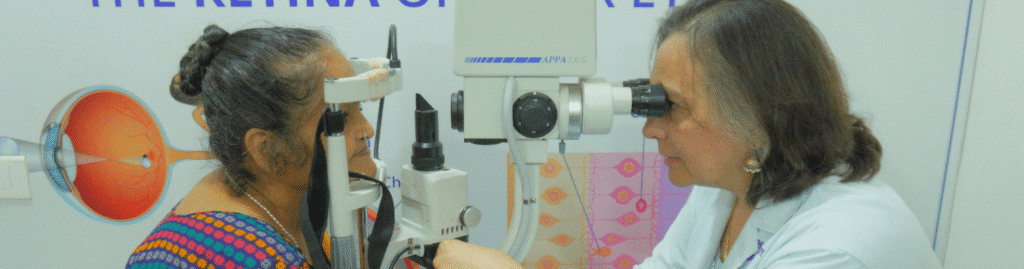
Glaucoma diagnosis begins with a comprehensive examination of ocular health, including the use of
- Tonometry: Tonometry is used to assess the internal pressure of the eye.
- Pachymetry: Pachymetry measures corneal thickness, which influences ocular pressure readings.
- Visual Field Test: The Visual Field Test is used to assess loss of peripheral vision and, at the same time, determine if you have blind spots (called scotoma).
- Fundus Examination: Focuses on observing the optic nerve.
- Optical Coherence Tomography (OCT): Offers high-resolution images of the optic nerve and retina, uncovering subtle indicators of Glaucoma. Ask ChatGPT
These diagnostic tools are crucial for early detection, personalised treatment plans, and practical vision preservation.
Understanding Glaucoma: A Comprehensive Management Plan
A lifetime commitment to treatment:
Glaucoma, the ‘Silent Thief of Sight’ requires ongoing check-ups and vigilance. It hides and can cause irreparable vision loss if not examined and treated. The primary approach to treatment often includes the use of doctor-prescribed eye drops. These eye drops reduce Intraocular Pressure (IOP), preventing disease and protecting vision.
Regular Monitoring and Adjustment:
Patients with Glaucoma must undergo check-ups every 3 to 6 months to ensure consistent care. These regular visits are crucial for evaluating the effectiveness of the treatment and implementing any required adjustments. Constant monitoring enables the early detection of changes in the condition.
Advanced Treatment Options:
Treatment for Angle-closure Glaucoma may involve a range of extensive interventions. Laser Peripheral Iridotomy creates a small opening in the iris to lower Intraocular Pressure (IOP). The space improves the outflow of water-based fluid, effectively minimising eye pressure.
Surgical Considerations:
Surgical options, like Trabeculectomy, may be considered when medication and laser treatments cannot manage ocular pressure. The procedure aims to create a new channel for fluid drainage, thereby lowering Intraocular Pressure and mitigating the risk of further optic nerve damage. Such operations are crucial for individuals who do not respond well to less invasive therapy.
The Importance of Early Detection:
Early screening and proper diagnosis in Glaucoma treatment cannot be emphasised enough. Early detection is critical to initiating effective treatment strategies and preventing significant vision loss. Regular eye examinations are essential for discovering Glaucoma in its initial stages and enhancing its management and prognosis.
Conclusion
Glaucoma management requires early discovery, regular monitoring, and medication adherence. Regular eye exams detect the condition early, while individualised treatment plans slow growth. Consistently following instructions from Ophthalmologists can help Glaucoma patients control their eye condition and prevent blindness. Since Glaucoma is a “Silent Thief of Sight”, Make sure to detect it early with a yearly eye check.
Refer to the blog for further information on the Importance of early Glaucoma Detection.
We at Zamindar Micro Surgical Eye Care Center have a dedicated Glaucoma Clinic focusing on screening, early detection, treatment, and systematic follow-up of Glaucoma patients.
watch full video here: Why Is Glaucoma Called The Silent Thief Of Sight By Dr Priya Timothy